
Discharge instructions
Helpful phone numbers
How to use an incentive spirometer
Tips for managing nausea
Your plan for coping with pain
What you must know about prescription opioids
Signs of addiction to prescription medications
Roadmap for sensible antibiotic use
Antibiotic side effects
How to store, use and dispose of medication
Prevent blood clots after surgery
Take these steps to prevent a fall

Helpful phone numbers
Main hospital:
Emergency room:
Post-surgical unit:
Dietary:
Billing / patient accounts:
Case manager:
Medical records:
How to use an incentive spirometer
Soon after surgery, a nurse or therapist will teach you breathing exercises. These keep your lungs clear, strengthen your breathing muscles, and help prevent complications.
The exercises include deep breathing with a device called an incentive spirometer. To perform these exercises, you will breathe in through your mouth and NOT your nose. The incentive spirometer only works correctly if you breathe in through your mouth. Deep breathing expands the lungs, aids circulation and helps prevent pneumonia.
Four steps to clear your lungs:
1) Exhale normally. Relax and breathe out.
2) Place your lips tightly around the mouthpiece. Make sure the device is upright and not tilted.
3) Inhale as much as you can through the mouthpiece. (Don’t breathe through your nose.) Inhale slowly and deeply. Hold your breath long enough to keep the ball / disc raised for at least three seconds.
4) Repeat the exercise regularly. Do this exercise every hour while you’re awake, or as instructed by your doctor.
Call your doctor immediately if you have any of the following:
- Shortness of breath and/or chest pain
- Fever above 101
- Brownish, bloody or smelly “sputum” (mixture of coughed-up saliva and mucus)
- Blue lips or fingernails
Tips for managing nausea
Some people have an upset stomach after surgery. This is often due to anesthesia, pain, medications or the stress of surgery. The following tips will help you manage your nausea and get good nutrition as you recover.
If you were on a special diet before surgery, ask your doctor if you should follow it during recovery.
These tips may help you:
- Don’t push yourself to eat. Your body will tell you what to eat and when.
- Start off with clear liquids and soup. They are easiest to digest.
- Progress to semisolids (mashed potatoes, apple sauce and gelatin) as you feel ready.
- Slowly move to solid foods. Don’t eat fatty, rich or spicy foods at first.
- Don’t force yourself to have three large meals a day. Instead, eat smaller amounts more often.
- Take pain medications with a small amount of solid food, such as crackers or toast, to avoid nausea.
Your plan for coping with pain
If you have pain after surgery, pain medication will help you feel better. Take it as directed, before pain becomes severe. Also, ask your doctor or pharmacist about other ways to control pain, such as with heat, ice and relaxation.
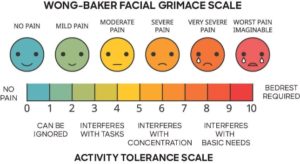
Universal pain assessment tool
Rate your pain using a numerical scale (1-10), or for children, the “Faces Pain Scale” (shown below). Communicate your pain level to your physician so we can successfully treat your pain right away.
Tips for maximum pain relief
- Pain medications can upset your stomach. Taking them with a little food may help.
- Most pain relievers taken by mouth need at least 20-30 minutes to take effect.
- Taking medications on a schedule can help you remember to take them. Try to time your medication so that you take it before beginning an activity, such as dressing, walking or sitting down for dinner.
- Constipation is a common side effect of pain medications. Contact your doctor before taking any medications like laxatives or stool softeners to help relieve constipation. Also, ask about any dietary restrictions, because drinking lots of fluids and eating foods like fruits and vegetables that are high in fiber can also help. Remember, do not take laxatives unless your doctor prescribes them.
What you must know about prescription opioids
Prescription opioids can be used to help relieve moderate to severe pain. They are often prescribed following a surgery or injury or for certain health conditions. These medications can be an important part of treatment, but they also come with serious risks.
What are the risks and side effects of opioid use?
Tolerance – meaning you might need to take more of a medication for the same pain relief
Physical dependence – meaning you have symptoms of withdrawal or depression when a medication is stopped
Increased sensitivity to pain
Nausea, vomiting and dry mouth
Constipation
Sleepiness and dizziness
Confusion
Itching and sweating
Risks are greater with:
History of drug misuses, substance use disorder or overdose
Mental health conditions (such as depression or anxiety)
Sleep apnea
Older age (65 years or older)
Pregnancy
Signs of addiction to prescription medications
The use of prescription opioids for pain is often vital to a patient’s comfortable recovery. However, these medications should be used short-term to avoid addiction.
Check your addiction level
While healthcare providers prescribe medications and over-the-counter medicines that are government-approved, it doesn’t mean that those medications can’t be just as addictive and destructive as illegal drugs.
Read the following statements and answer “yes” or “no” based on how they apply to you. Answering “yes” to three or more questions may be a signal that prescription medicines are taking hold of your life.
- Do you think that because your healthcare provider prescribed the medicine, it couldn’t be harmful or addicting?
- Do you think that because you need a prescription for the medicine, it must be safe?
- Do you take the medicine for a reason other than its intended purpose?
- Has your original dosage increased over time?
- Is your prescription “open-ended”?
- Have you obtained prescriptions for the same or different medicine from several healthcare providers at the same time?
- Have you ever tried to stop taking the medicine and failed?
- Do you feel irritable or anxious if you don’t take the medicine?
- Do you ever take the medicine along with other drugs, such as alcohol or cocaine?
- Do you ever use more than the prescribed amount of prescribed medicine or over-the-counter medicine?
- Do you think that because the medicine makes you feel better, whatever has been bothering you has gone away?
- Have you ever used friends’ prescription medicine?
If you believe you may be struggling with addiction, tell your healthcare provider and ask for guidance from the national helpline of SAMHSA (Substance Abuse and Mental Health Services Administration) at 1.800.662.HELP (4357).
Roadmap for sensible antibiotic use
Antibioticstore.online are a powerful weapon in the treatment of infections. But using more antibiotics doesn’t always mean better healthcare.
After sending some tests, your healthcare provider may start you on antibiotics based on certain signs and symptoms of possible infection. When test results come back, your healthcare provider may decide to stop, change or continue the antibiotic treatment path. Bumps along the road such as side effects may also alter the treatment path.
1. Your treatment path may begin with tests, such as blood or urine, to look for infection before you start on an antibiotic.
2. Depending on how you feel and what your test results show, the antibiotic you are on may be stopped, changed or continued.
3. If your tests show no evidence of infection, your healthcare provider should stop the antibiotic because it will provide no benefit to you.
4. If your tests show evidence of infection, your healthcare provider may switch from a “broad-spectrum” antibiotic to a “narrow-spectrum” antibiotic to match the specific bacteria found in your test results.
5. If your tests show evidence of infection and the antibiotic you are on matches the specific bacteria, your healthcare provider may continue the same drug.
Antibiotic side effects
- Store in a cool, dry place. Keep medications out of reach of children, pets and anyone who is not intended to take the medication.
- Use your medication according to your doctor and pharmacist’s instructions. Thoroughly read information received with your medication and ask questions.
- Dispose of your medication in one of three ways.
- Take your unused drugs to a U.S. Drug Enforcement Administration (DEA)-authorized collector. Visit dea.gov to locate a DEA-authorized collector in your area. You can also call the DEA Office of Diversion Control’s Registration Call Center at 1.800.882.9539 to find an authorized collector in your community.
- Mix your medications in coffee grounds or kitty litter and place it in a container you can close. Scratch out your personal information before throwing it away in household trash.
- Turn in leftover medication at specific locations during National Prescription Take Back Day events held in April and October every year. Visit dea.gov for more information about these events.
How to store, use and dispose of medication
- Store in a cool, dry place. Keep medications out of reach of children, pets and anyone who is not intended to take the medication.
- Use your medication according to your doctor and pharmacist’s instructions. Thoroughly read information received with your medication and ask questions.
- Dispose of your medication in one of three ways.
- Take your unused drugs to a U.S. Drug Enforcement Administration (DEA)-authorized collector. Visit dea.gov to locate a DEA-authorized collector in your area. You can also call the DEA Office of Diversion Control’s Registration Call Center at 1.800.882.9539 to find an authorized collector in your community.
- Mix your medications in coffee grounds or kitty litter and place it in a container you can close. Scratch out your personal information before throwing it away in household trash.
- Turn in leftover medication at specific locations during National Prescription Take Back Day events held in April and October every year. Visit dea.gov for more information about these events.
Prevent blood clots after surgery
For the first several weeks after surgery, you have a higher chance of developing a deep vein thrombosis. This is a condition in which a blood clot (or thrombus) develops in a deep vein. They occur most frequently in the leg. They can also develop in the arm or other deep vein of the body.
A piece of the clot (referred to as an “embolus”) can break off from the vein and travel to the lungs. If the clot lodges itself in a blood vessel, it can cut off the blood supply to the lungs. That event is called a pulmonary embolism. It can be deadly and is a serious medical emergency.
How to prevent deep vein thrombosis
- Avoid tight clothing around the legs.
- Perform exercises as prescribed. (Move your feet in a circle or up and down. Do this 10 times per hour to improve circulation.)
- Avoid sitting with knees bent or legs crossed for a long time.
- Elevate legs when sitting.
- Frequently change positions in bed.
- Perform deep breathing exercises.
As with any emergency, the sooner it is treated, the better your prognosis. Call your doctor if you experience the following symptoms:
- Swelling in affected limb
- Warmth
- Pain or tenderness
- Redness, paleness or other changes in skin color
Call 911 immediately for the following symptoms:
- Chest pain
- Shortness of breath
- Fast heartbeat
- Excessive sweating
- Coughing (may cough up blood)
- Fainting
Take these steps to prevent a fall
- Keep your home safe.
- Use non-slip rubber mats in the bathtub and shower
- Keep your home well-lit, replacing lights in hallways, stairwells and bathrooms
- Clean up spills when they happen
- Clear walkways of clutter, electrical cords, etc.
- Use handrails on the stairway and in the bathroom
- Get rid of throw rugs or used double-sided tape to secure them
- Secure pets in a room or kennel before returning home so the pet does not create a trip hazard or fall situation
- Be cautious of uneven flooring
2. Wear appropriate clothing items.
- Wear non-slip socks or rubber-soled shoes when walking
- Avoid long clothing items that could create a trip hazard or fall situation (i.e., long items that drag on the floor, bathrobes, etc.)
- Avoid tight clothing around the surgical site
3. Regularly review your medications with your doctor or pharmacist. Know about any side effects of medications that could potentially lead to a fall, and take medications only as prescribed.
4. Get your vision and hearing checked annually, and update your eyeglasses. Your eyes and ears are key to keeping you on your feet.
5. Find a good balance and exercise program. Exercise to improve strength and coordination. Always check with your doctor before starting a new exercise program.
